Most health care providers agree that the overwhelming issue they currently face is staff retention and recruitment. The American Hospital Association recently called the workforce shortage that hospitals are experiencing a “national emergency,” projecting the overall shortage of nurses to reach 1.1 million by the end of the year.
The situation is only getting worse. A 2022 Elsevier Health survey found that 47% of U.S. health care workers plan to leave their current role within the next two to three years.
The solutions seem obvious: new approaches to training, better pay and career opportunities, recruiting more workers who face barriers to employment, and promoting the mental wellbeing of frontline workers. But these are not quick fixes and are not easy to achieve, particularly in light of current economic pressures.
In the meantime, the vacancy gap puts added pressure on existing staff, some of whom will then leave, thus increasing the vacancies. The cycle is plain as day.
Turning to technology
Technology in the workplace has the power to attract and retain employees in every industry, including health care. A January 2022 survey of 9,600 frontline health care workers from Microsoft’s Work Trend Index found that 63% of respondents are “excited about the job opportunities (that) tech creates.” Respondents ranked technology tools third among 12 potential factors that could reduce workplace stress.
The message was clear. And too often, behavioral health providers lag behind technologically. But the tide is turning, with help from UK-based Oxehealth.
Oxehealth’s Oxevision is an innovative vision-based patient monitoring system that enables staff in behavioral health facilities to measure patients’ pulse and breathing rate remotely and completely contact-free. It is already being used by half of English NHS behavioral health providers to improve safety and care quality, with the added benefit of improving the experiences of the staff who use it.
Making the day-to-day less stressful
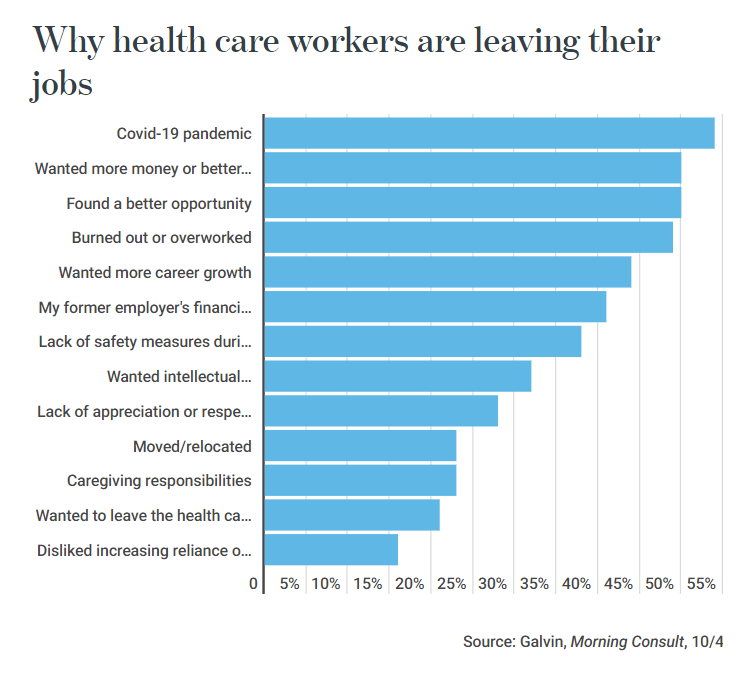
While there are many reasons why staff leave health care jobs, burnout plays a significant role. Leveraging vision-based patient monitoring technology like Oxevision can help curb work-related stress. The system supports staff to preserve the physical health of their patients, helping to prevent serious incidents from occurring.
In a staff survey carried out with some of Oxehealth’s UK partners, 94% of respondents said Oxevision helped them to improve patient safety, while 85% felt better able to manage patient risk.
“Night time is seen as the highest risk time as there are fewer staff on shift and they can feel a little isolated,” says one unit manager at a UK behavioral health hospital that has deployed Oxevision. “Now staff have the ability to check on patients using the system. It provides that reassurance to nursing staff which in turn decreases their anxiety.”
Staff in behavioral health facilities can and do encounter hostility, aggression and assault at work. The ability to monitor patients remotely at night and in high-risk situations can reduce such encounters while minimizing disturbance to patients: in the multi-site Oxehealth survey, 73% of staff reported that Oxevision helps them to manage their own safety.
Boosting efficiency through smarter rounding
Without vision-based patient monitoring technology, Q15 rounding is deeply disruptive to patients, because staff members have to open bedroom doors to check patients’ wellbeing. It is also extremely time-consuming. Carrying out checks every 15 minutes equals almost 100 observations for just one patient in a 24-hour period.
Digitally assisted nursing observations with a vision-based patient monitoring system enable staff to check the welfare of all their patients from one computer or tablet, saving time that would normally be spent walking up and down the unit. This is possible because vital sign measurements are obtained at medical grade accuracy.
Unsurprisingly, Oxevision-supported observations have been found to take almost half of the time that conventional observations take. This smarter rounding boosts efficiency and frees up time for staff to get on with other duties, like engaging with patients therapeutically and reacting quickly when the unexpected happens. Their time on the job is better spent. Their confidence is higher. Their experience is better. And retention improves.
“The system is part of our team,” says Laura Fitzpatrick, a unit manager of behavioral health provider Coventry and Warwickshire Partnership NHS Trust, that works with Oxehealth. “It’s our 6th team member of staff on the night shift. It cannot do the hands-on care, but it can give you more time [for the hands-on care].”
Supporting rounding with additional physiological data that otherwise wouldn’t be available can also reduce the need for patients to be on one-on-one observations. This means fewer agency staff which, at a time when there’s a critical shortage of nurses, has important implications for behavioral health providers.
And important implications for patients, too.
“I couldn’t imagine not having the system now in place,” says Tracey Wench, executive director of nursing and quality at one of Oxehealth’s partner providers. “It’s something that makes us feel more secure and we feel it sets up safety for the patients.”
To learn more about how Oxevision can help your patients and staff, visit Oxehealth.com.
This content was originally published in Behavioral Health Business on 9 December 2022: https://bhbusiness.com/2022/12/09/how-behavioral-health-providers-can-tackle-staffing-issues-with-technology/





