Company History & Evolution
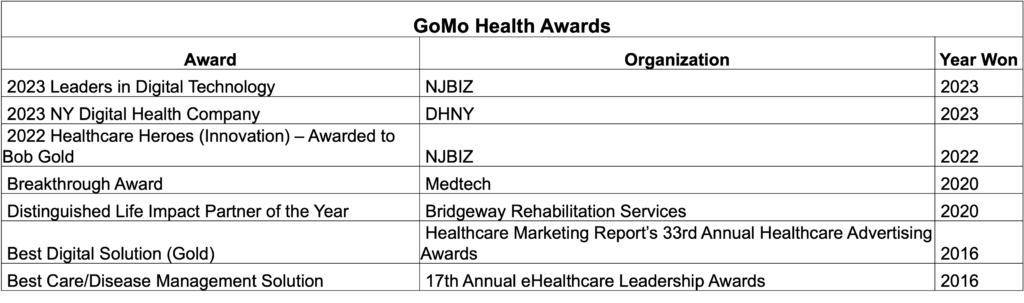
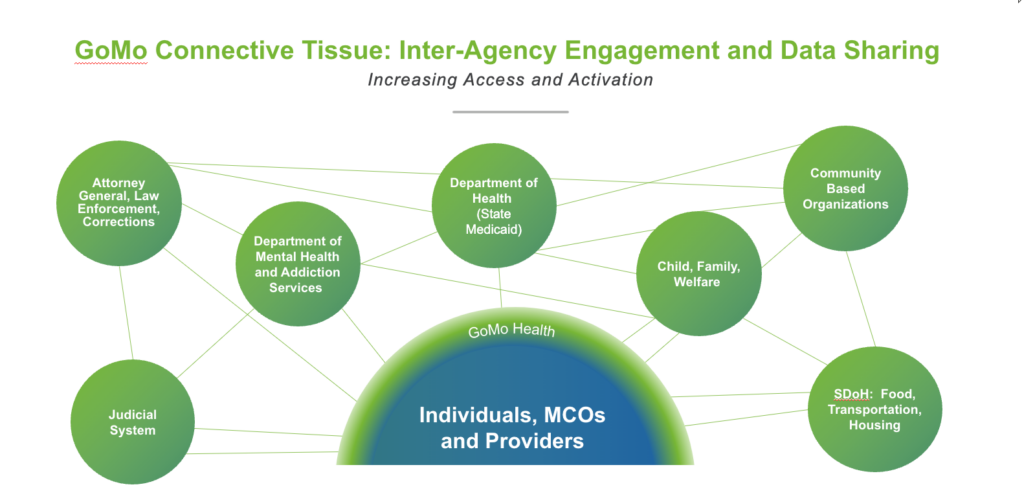
GoMo Health was established in 2013. Leveraging years of applied research in the “digital-to-human” behavioral and cognitive science of human motivation, activation, and resiliency, Bob Gold, Chief Behavioral Technologist and Founder, began applying BehavioralRx®, his (then) emerging digital therapeutic engagement science to engage with millions of underserved and vulnerable patients, caregivers, and families with mental health challenges ranging from anxiety and depression to mental illness, developmental challenges such as pediatric autism, and substance use. Today, because this behavior modification engagement science is evidence-based, it is used globally by federal/state health organizations, health plans, hospitals, providers, employers, and life sciences companies to produce measurably better health outcomes, increased adherence, retention and satisfaction, and significantly reduced cost of care.
An important design capability is the ability to scale and reach millions of lives – via that country’s telecommunications and mobile network of which GoMo has established interfaces to most wireless carriers. Equally as important is the ability to scale cost-effectively, ranging from a couple of U.S. dollars per patient/per month down to pennies on the dollar at massive scale.
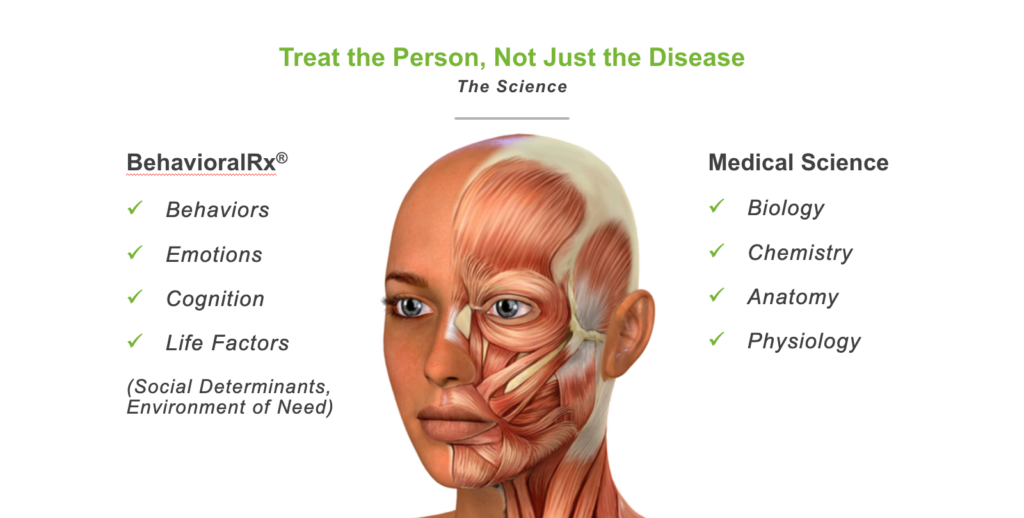
Our differentiator? BehavioralRx. Based on the principle that no two people are alike, therefore, neither can be their care management, our (now) evidence-based science drives the award-winning personalized engagements that we create and deliver.
Considering a whole person approach to care, addressing physical and psychosocial needs, our “bot” interacts with patients to assess their “environmental factors” – including confidence in ability to follow their care plan and “life factors” outside of clinical diagnosis that are to be considered and addressed to ensure a successful “whole person” health management engagement. Our system, the GoMo platform, maintains ongoing (cloud based – no app to download) touch points with program participants to track individual needs and deliver resources accordingly, with the ability to pivot deliverables and support changing patient needs and priorities.
Program Use Case: The Rimrock Foundation – Recovery Pathways
Digital Therapeutic Increases Success of Behavioral Health Treatment Programs
Rimrock, the largest treatment center for adults with substance use and co-occurring disorders in Montana, views addiction as a whole person illness, affecting an individual’s emotional, physical, spiritual, and social wellbeing.
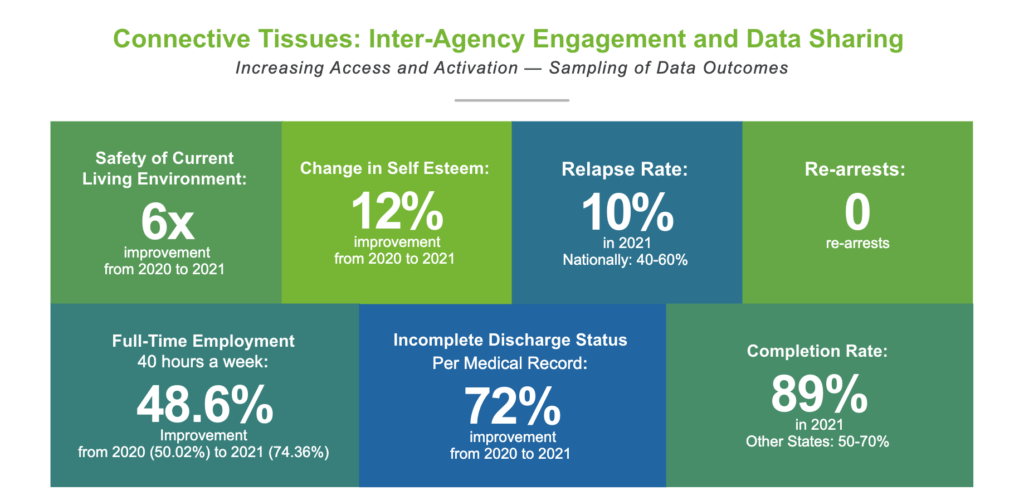
GoMo Health collaborated with Rimrock to create and deliver Recovery Pathways, a personalized engagement solution for justice-involved participants from seven different treatment courts. The program’s success led to Rimrock adapting it for use in all outpatient substance use disorder and mental health treatment programs.
Program Goals
For Members:
- Address social determinants of health that are barriers to recovery
- Reinforce therapies outside of program sessions
- Reduce member relapse rate
- Increase program completion rates
For Support Persons:
- Provide behavioral and emotional support
- Share proven tactics for engaging with member in program
- Increase empathy for loved ones in the program
- Increase appropriate boundary-setting
BehavioralRx®, The Science of Precision Health
GoMo Health leveraged its proprietary emerging science, BehavioralRx, to build the program and determine the engagement strategy, approach and content delivered.

The following behavioral and cognitive techniques were applied:
- Reduction Technology / Persuading through simplifying.
- Tailoring Technology / Persuasion through customization.
- Nurturing Technology / Guided persuasion.
- Conditioning Technology / Reinforcing target behavior.
- Environment of Need Technology / Intervening at the right time.
A Whole Person Approach to Addiction Treatment
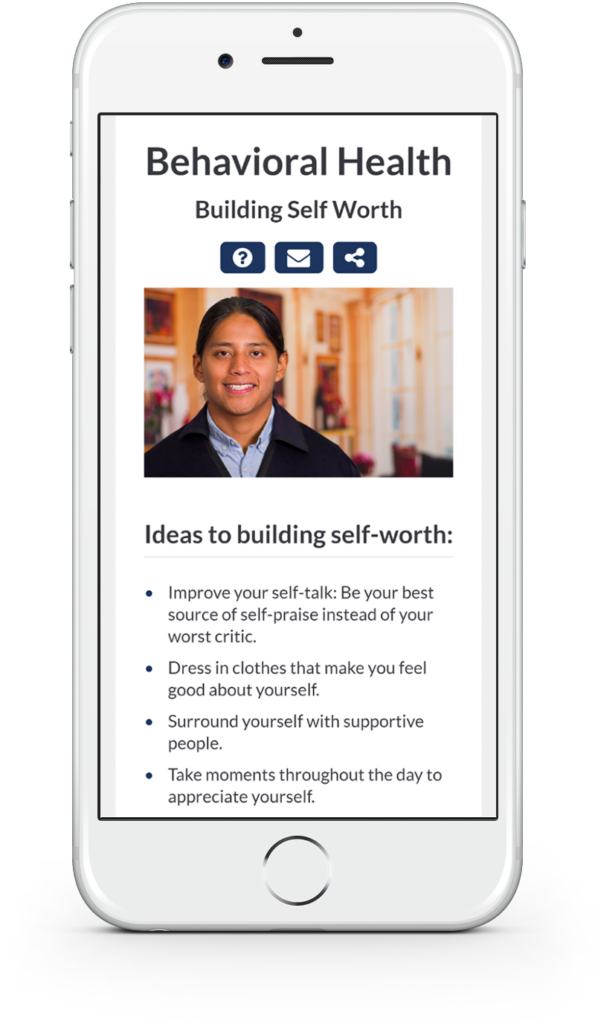
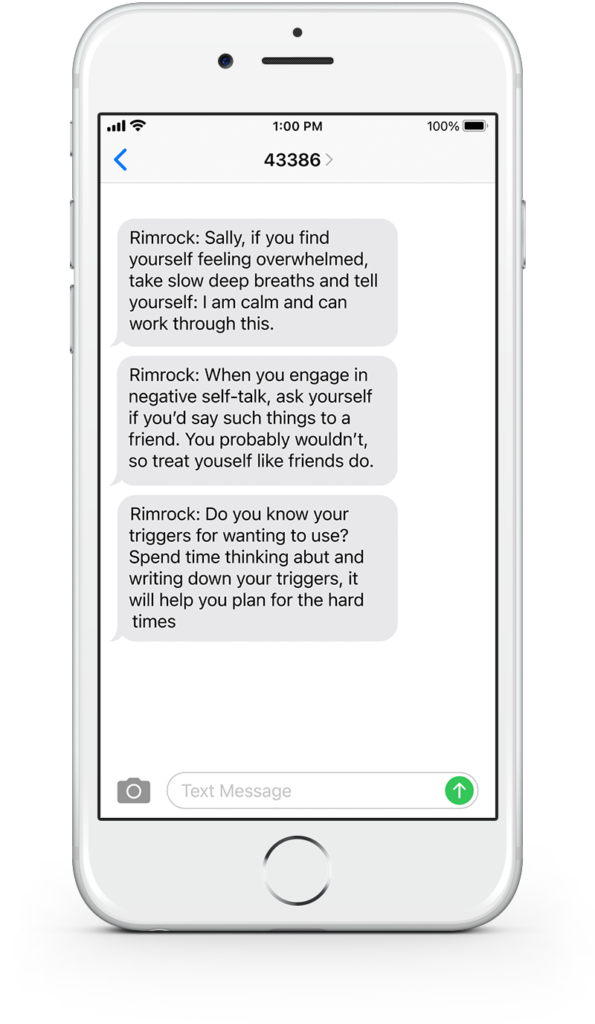
Core to the program is the understanding that patients are first and foremost, human and takes into account circumstances and lifestyle outside of the treatment setting. Participants receive a regular cadence of personalized content, care messages, surveys, and bi-directional chat to motivate and inspire them along their treatment journey and deliver what they need, in the moment they need it. To extend the impact, the program continues even after completion of treatment, providing ongoing support for up to a year.
Content includes:
- Coping skills
- Shame resiliency
- Self-care/mindfulness
- Handling independence
- Preparing for court
- Music behavioral engagement
Research has continued to show the importance of strong support systems for addiction recovery.
The Recovery Pathways program was built with additional content specific to support persons. Once enrolled, participants are also able to include a loved one/support person into the program to receive content specific to their role as caregiver.
Content Customization and Personalization
Message tracks are customized by several characteristics of the participant or support person, including whether they are a parent and age of child(ren), where they are in their journey, and their type of treatment court.
Court Tracks
Seven treatment courts are supported:
- Co-occurring Court
- Family Recovery Court
- Felony DUI Court (STEER)
- ICWA Court
- Misdemeanor Court
- Pilot Court
- Veteran Court (CAMO)
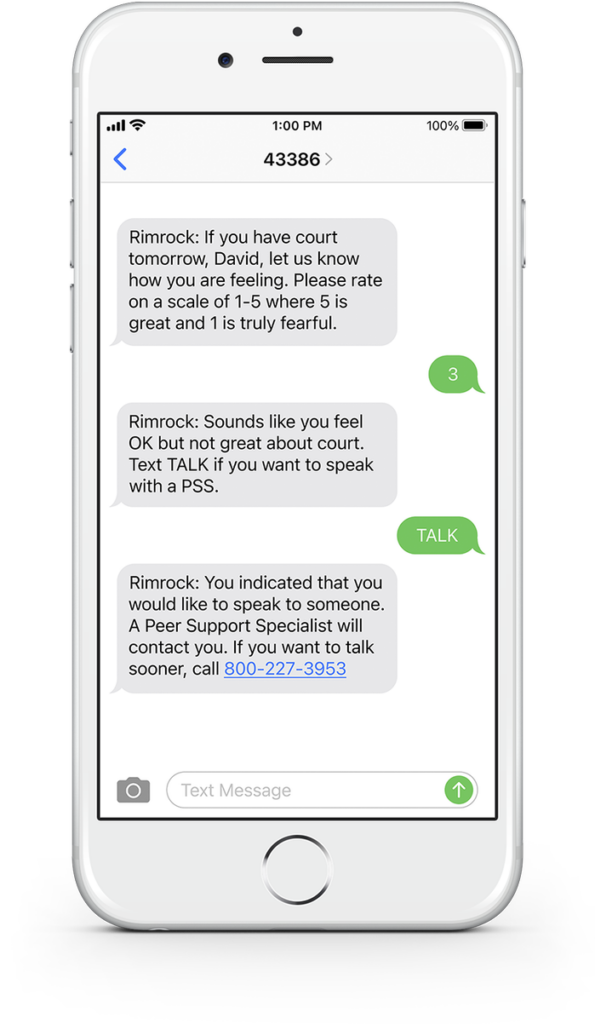
In addition to the Care Messages, participants can reach out for help when and where they need it.
All participants can text in any of the following keywords at any time to receive an in- the-moment message of support:
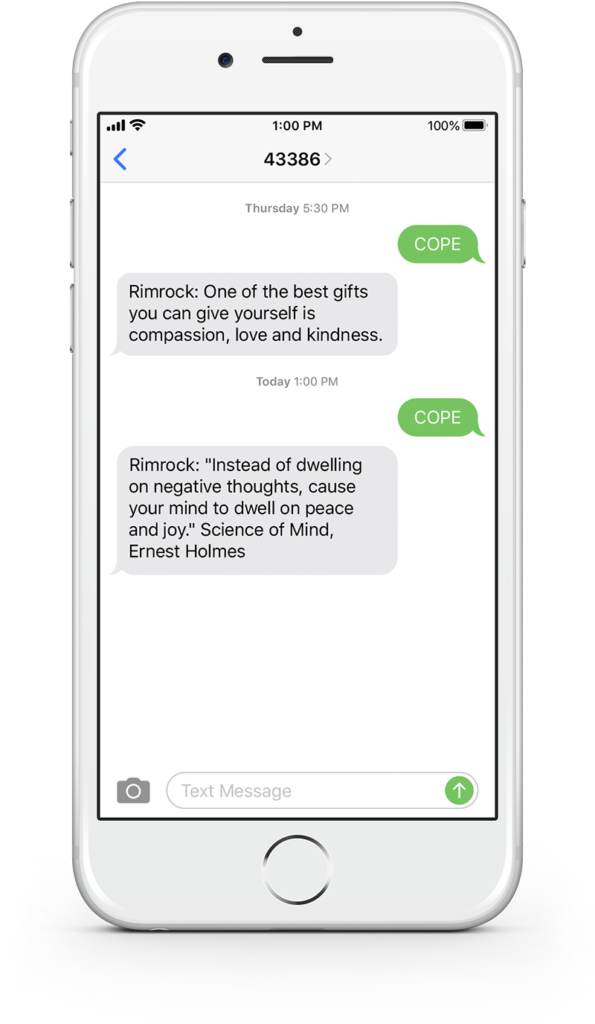
- COPE – Coping strategies and content related to thinking errors
- PEER – A story/video from other people who have shared similar experiences
- SMILE – A joke or uplifting content
- SUPPORT – Link to a resource guide that includes local resources for legal services, AA meetings, and more
- TALK – To request help from a Rimrock peer support specialist
- MUSIC – To help with hope and healing
- IDEA – To submit helpful tips or positive motivation to support others
Addressing Addiction Among Native Americans
While Native Americans account for only a small part of the U.S. population (about 1.7%), they experience much higher rates of substance use compared to other racial and/or ethnic groups.
Factors that contribute to this increased risk include historical trauma, racism, lack of health insurance, poverty, and more.
- 25% of enrolled program participants are Native American
- 14% of all participants have expressed interest in Native
American-specific content, 80% of whom are enrolled members of a tribe