“It’s the happiest time in your life!” “Enjoy every moment!” “It goes by so fast!” These are common heartfelt words shared with new moms. But what happens when it’s not the happiest time, when it’s impossible to enjoy just about any moment, and when time not only doesn’t fly by but seems to stand still? For approximately 20% of moms who face postpartum depression (PPD) (closer to 40% among women of color and/or those suffering from other physical or mental health conditions), these societal expectations of joy and the directive to “savor this special experience” may make an already dark time feel even more desolate.
The inherently isolating condition of PPD is exacerbated by the fact that no two depressive episodes or people are exactly alike, but they do share a common theme. All depressions paralyze the very part of the sufferer that is needed to heal. The apathy, lack of motivation, and sheer exhaustion require that someone—or something other than the person in the grip of the disease—take the first step toward healing. Help is needed in order to verbalize that there is an issue, to reach out for help, make a call, schedule an appointment, and most importantly, decide that something must change. This realization that those suffering from PPD need help, compels the effort needed to put the desire for change into action. All too often, people suffer in silence, neither asking for help nor waving a flag, so the disease remains invisible and destructive. This is where support and intervention are necessary to get people the help they need. Mental health management will always require some form of human care, compassion, and skill, but there are ways that technology can enhance and extend human reach.
GoMo Health has been able to help people worldwide with the management of multiple chronic conditions, including postpartum women with depression. Our cloud-based system, the GoMo Platform, maintains ongoing touchpoints with program participants to track their needs and deliver resources accordingly. GoMo Health offers the ability to pivot support to mirror changing priorities and electronically triage and escalate those needs to the providers (when necessary). The providers can then connect directly with those who are suffering, enabling support in moments of need. This ensures that no one suffers in silence, and in this case, that moms with PPD are cared for so that they truly can “enjoy every moment” and feel that they are living the “happiest time of their life.”
Below are three examples of perinatal programs that GoMo Health has created in conjunction with our client partners to support the mental health of pregnant and postpartum moms. Each has distinct physical health and programmatic objectives, but all focus on mental health and psychosocial well-being as well.
WellCare of Nebraska Baby’s First Program:
WellCare, a large Medicaid plan in Nebraska, partnered with GoMo Health to create the Baby’s First program to help new parents and caregivers, statewide, understand and track early-childhood development milestones, home safety, and how to cope emotionally as new parents. The creators of this program understood that a mom suffering from mental health issues would not be able to engage with the program or help their newborn effectively before their own needs were addressed. Understanding that mental wellness is achieved and maintained with a consistent focus, this program supported all new parents with their emotional needs and titrated the content and resources to ensure that everyone was “met where they were”—across the spectrum from having ‘normal’ adjustment struggles, based on the massive life change that a newborn brings, to meeting clinical criteria for a major depressive episode.
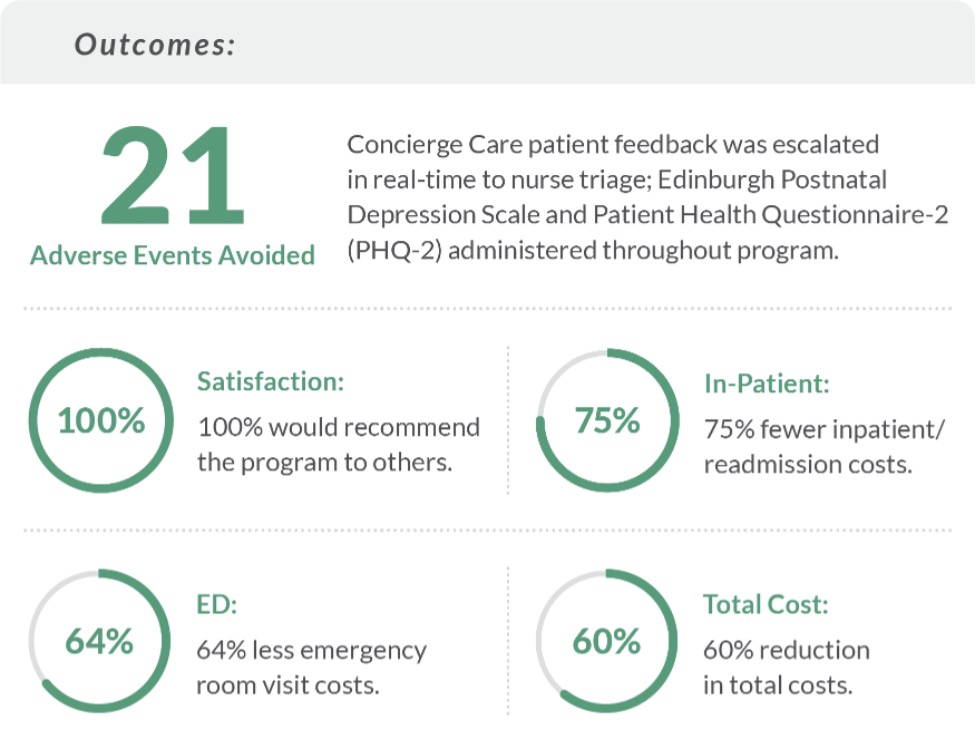
All participants received bi-directional Care Messages™, or SMS texts, simulating how a human would provide information and resources. All participants were administered the Patient Health Questionnaire-2 (PHQ-2) mental health screening. Based on participant responses to these two questions (commonly used by providers to triage the need to administer more in-depth depression screens), some participants were sent a link to complete the Edinburgh Postpartum Depression Scale. Nurse triage received real-time escalation notifications via email for those who had clinically significant scores. In doing so, the digital GoMo Platform successfully escalated 21 adverse events to nurse triage for immediate response.

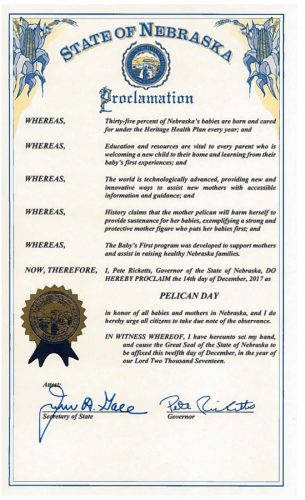
These escalations, along with the supportive content delivered, contributed to the program’s overall success as demonstrated by a 75% reduction in costs associated with inpatient visits and readmissions, a 64% reduction in costs associated with ED visits, and a 60% reduction in the overall total cost of healthcare for the population enrolled in the program. The outcomes were so impressive that Governor Pete Ricketts declared December 14, 2017 “Pelican Day” in Nebraska, urging all new parents to access resources like WellCare’s Baby First program for information to help raise healthy babies. The day was designated in reference to ‘pelican mothers’ who are known to pierce their own skin in order to save and provide nourishment to their starving babies—forsaking themselves in the process.
The Aga Khan Hospital Pre and Postnatal Concierge Program
The Aga Khan Hospital (in Africa) is yet another application of the GoMo Platform that highlights the benefits of the logic-based digital therapeutic during the prenatal period (in addition to the postpartum period). Highlighting the importance of telehealth in its ability to serve rural populations, this program supports pregnant women who visit The Aga Khan Hospital facilities. The project was designed to serve as a virtual care coordinator to remotely support expectant mothers through all stages of their journey. The objective was to reduce pre-term birth rates, risk of complications, ED usage, and overall costs of care delivery, as well as to improve overall maternal and child health.
As with the Baby’s First program, mental health was addressed through all phases of the journey, with consistent mental wellness check-ins as a cornerstone of the program. The PHQ-2 and the Edinburgh scales were used to screen for both prenatal and postpartum depression and to provide real-time communications/alerts back to the provider. In the first year of the program, providers received 15 escalations (notifications when clinically significant scores were recorded for the PHQ-2 and Edinburgh) based on feedback from the 172 engaged participants. Clinicians found this invaluable, given that they do not typically see the patients in-clinic with the frequency needed to keep current on their mental health status.
The program has boasted impressive results—reducing the preterm birth rate (to 1% compared to the national average of 12%) and proving valuable to the patients in their care journey: 100% of all program participants confirmed that the concierge program helped them better manage their health and pregnancy and that they would refer the program to a friend. When completing the prenatal portion of the program, 77% desired to continue with the postpartum component of the program.
Mom’s Heart Matters
Originally created to reduce rates of maternal mortality associated with preeclampsia and hypertension among postpartum Black women in Georgia, Mom’s Heart Matters is a collaboration between Amerigroup, Georgia Family Connection Partnership, Georgia OBGYN Society, Morehouse School of Medicine, and the Annie E. Casey Foundation. Focused on postpartum cardiovascular wellness, the program utilizes remote patient monitoring with Bluetooth® connected blood pressure cuffs; but because of the high rates of comorbid PPD associated with these cardiovascular conditions, the program addresses maternal mental health as well. Addressing cardiovascular health and mental health conditions simultaneously is crucial given that a mother struggling in the throes of a depressive episode would likely be both mentally and physically unable to focus on or engage in the health care behaviors required to ensure she thrives despite her cardiovascular diagnosis.
As with the first two programs highlighted, all participants in the Mom’s Heart Matters program receive bi-directional Care Messages™, or SMS texts, as well as requests to complete the Patient Health Questionnaire-2 (PHQ-2) screening, simulating how a human would administer the survey. Based on how a participant responds to these two questions, they may receive a link to complete the full Patient Health Questionnaire-9 (PHQ-9) depression scale. Clinically significant scores trigger an escalation to the provider, notifying them that their patient is at risk for depression and/or suicide. The provider can then reach out to assist the participant immediately. This helps the patient in real-time, based on their self-expressed needs, and leverages the power of technology to scale the support of the clinical care team.
In addition to the PHQ-2 and 9, participants are also pulsed The Barkin Index of Maternal Functioning (a 20-item, self-report questionnaire that assesses overall well-being in the context of motherhood). Keisha Callins, MD, MPH (OB/GYN and Clinical Assistant Professor at Mercer University School of Medicine and advisor to the project team that designed the Mom’s Heart Matters program) learned about the Barkin Index when working alongside Jennifer Barkin, PhD, at the Mercer University School of Medicine, Department of Community Health. “I was immediately intrigued with this patient-inspired assessment tool that really helps to identify opportunities for support and linkage to resources along the spectrum of challenges that new moms encounter in addition to depression and anxiety,” says Dr. Callins.
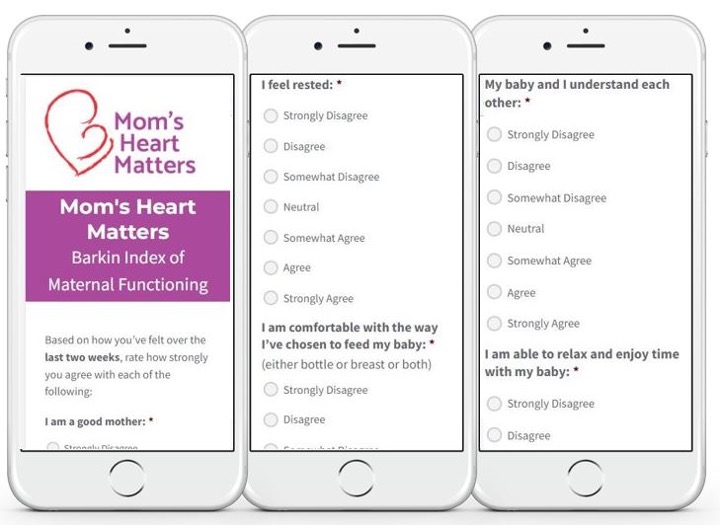
Patients who score even marginally on the PHQ-9 or the Barkin Index are automatically entered into an additional mental wellness support track in the program, through which they receive weekly reminders with bite-sized messages that include links to websites or content to incrementally support their mental well-being with the goal of long-term improvement.
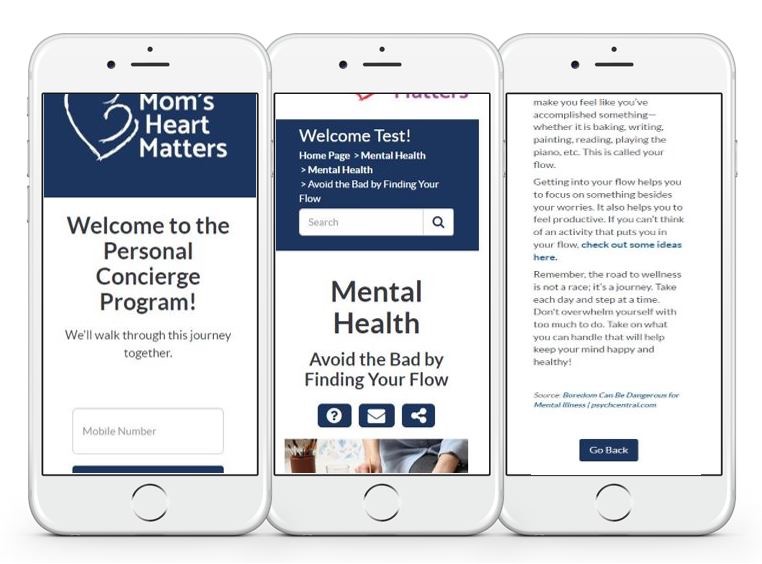
This program launched in January of 2023, so detailed outcomes data is not yet available, however, based on early process metrics, the program has been able to detect elevated blood pressures and concerning mental health signs and symptoms to escalate to providers and get help to moms immediately. According to Dr. Callins, “Mom’s Heart Matters is a unique initiative that intertwines a trusting clinician-patient relationship with an innovative technology platform to reinforce the safety net that every mom needs and deserves.”
Technology can never replace the healing potency of human connection—touch, compassion, and care—to ease physical or mental suffering, however, the success of the GoMo Platform to act as an extension of the human care team has proven invaluable. Clinicians often lament that they cannot go home with all their patients to be able to check on them constantly and provide them with real-time support, advice, and resources. This technology allows them to come as close to that as possible. Health care providers can leverage the technology to triage needs and deliver resources, while simultaneously gleaning information from all their patients and getting alerts to know who is immediately in need of human connection. A participant lucky enough to be supported by GoMo Health will never suffer alone.